Death is an inevitable part of life. Despite its certainty, it is often enveloped in silence and fear, leading to a reluctance to discuss it openly, even with loved ones. This hesitance can result in premature and extreme medical interventions, depriving patients of their dignity in their final days. Understanding and accepting death as a natural part of life allows individuals and their families to approach the end of life with dignity and peace.
Death Literacy
Death literacy goes beyond mere knowledge; it involves acceptance, compassion, and preparation for death. This includes familiarising oneself with the dying process, understanding the medical and legal aspects of end-of-life care, and recognizing the emotional and spiritual dimensions of death. Such awareness empowers individuals to make decisions that respect their lives, allowing families to fulfill their loved ones’ wishes during their final journey, free from unnecessary suffering and pain.

The Pain of Denial
Denial of death – and reluctance to discuss it – often leads to extreme treatments that do not reflect the patient’s true desire for a peaceful, dignified death. In India, terminally ill patients are commonly placed on life support systems in intensive care units (ICUs), where the goal is to prolong life at any cost. This can result in an impersonal, loveless death that the patient never wanted, depriving them of a dignified farewell in familiar surroundings or in the presence of loved ones.

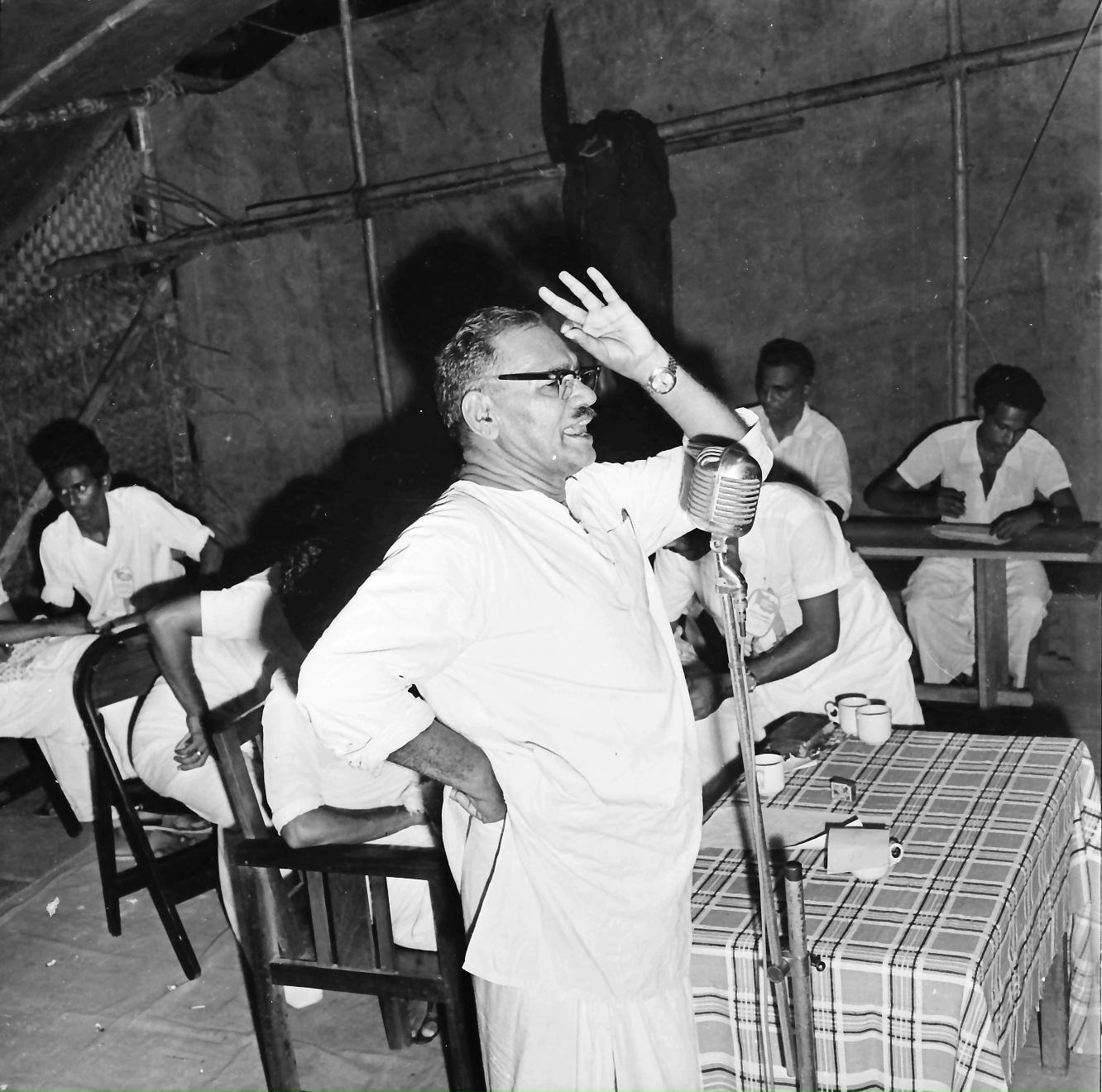
In a recent article in The Hindu, Dr. M.R. Rajagopal, one of the pioneering palliative care physicians in India, highlighted cultural differences in end-of-life care, comparing the deaths of former Indian Prime Minister Atal Bihari Vajpayee and ex-U.S President Ronald Reagan. Reagan, who died at home surrounded by loved ones, benefited from the West’s acceptance of advance care planning. In contrast, Vajpayee, bedridden for nine years after a stroke, died in an ICU surrounded by machines. This disparity underscores the lack of death literacy and the trend towards intensive medical interventions in India.
The Role of Compassionate Care
Medical professionals must lead the change by engaging in open and honest conversations with patients and their families about diagnoses and treatment options, especially in cases of untreatable cancer, comatose patients, and the elderly. This includes discussing palliative care treatments and the burdens of intensive treatment. Sometimes, the most compassionate choice is to allow a natural death.
Supporting patients in making informed decisions that align with their values and wishes ensures that care is not only medically sound but also deeply respectful of the patient’s dignity and humanity.
Legal and Ethical Requirements
A significant barrier to dignified end-of-life care in India is the lack of clear legal frameworks. The Supreme Court’s 2023 judgment allowing advance medical directives is a crucial step forward. However, widespread awareness and discussions are needed to ensure these directives are respected and followed.
Ethically, it is essential to recognize patient autonomy and their right to choose how to spend their final days. This includes the right to refuse intensive treatments and instead choose palliative care focused on reducing pain and suffering and improving the quality of life.
The Reality of Healthcare Decisions
Healthcare workers often face challenges in caring for dying patients in the ICU, concerned about medico-legal implications and the aggressive attitudes of relatives. Overcrowded hospitals may delay meeting patient needs, leading doctors to admit terminal patients to the ICU for round-the-clock care. However, this can deprive patients of the comfort of having their loved ones nearby.

In India, symptomatic treatments for terminally ill patients may not always be available at home, necessitating hospital visits. Clear communication between families and healthcare providers is crucial to ensuring the patient’s needs and wishes are met without undue stress or conflict.
Supporting Families in Grief and Decision-Making
The emotional and financial burden of end-of-life care decisions often falls on the patient’s loved ones. Without proper knowledge and support, they may opt for unnecessary treatments, believing it to be the best option. Social pressures from neighbors and distant relatives may influence these decisions. Educating families about death literacy can help them understand the natural course of terminal illness and the profound benefits of palliative care.
Intensive treatments that do not ensure the patient’s well-being can place a heavy financial burden on families and deprive them of the opportunity to care for their loved one in their final moments. Conversely, families who understand and accept death can better support their loved ones through a peaceful journey, often in the comfort of their own homes.
A Call to Compassionate Action
Promoting death literacy requires a multifaceted approach combining the efforts of medical professionals, policymakers, and educators to foster a culture where death is viewed not as a failure but as a natural end to life. This includes:
- Integrating Death Literacy into Medical Training: Ensure comprehensive training on palliative care and end-of-life discussions are included in the medical curriculum.
- Public Awareness Campaigns: Governments and NGOs should conduct campaigns to educate the public about the importance of advance directives and palliative care options.
- Support Systems for Families: Provide resources and support to help families navigate end-of-life decisions and compassionately care for their loved ones.
What is Advance Care Planning?
Advance care planning is an essential part of preparing for the end of life. It involves making decisions about the medical care you want if you become unable to communicate your wishes. This process includes documenting your preferences for specific treatments, such as life support or resuscitation efforts, and designating a trusted person, often called a healthcare proxy or power of attorney for healthcare, to make decisions on your behalf if necessary.

Why is Advance Care Planning Important?
- Ensures Your Wishes Are Followed: Having an advance care plan ensures that your medical preferences are documented and can be followed by healthcare providers, aligning care with your personal values and wishes.
- Reduces Stress for Your Family: In medical emergencies or serious illness, an advance care plan alleviates the burden on your family by clearly outlining your preferences, allowing them to focus on supporting you rather than making tough choices under pressure.
- Facilitates Clear Communication: An advance care plan promotes open conversations between you, your family, and your healthcare team about your desires and expectations, avoiding misunderstandings and ensuring everyone is on the same page regarding your care.
- Improves Quality of Life: By specifying your wishes, you can avoid unnecessary and possibly unwanted medical interventions, leading to a more comfortable and dignified end-of-life experience.
- Legal and Medical Guidance: Advance care plans often include legal documents, such as a living will or durable power of attorney for healthcare, providing clear instructions to healthcare providers and ensuring your healthcare proxy has the authority to make decisions according to your specified wishes.
How to Create an Advance Care Plan
- Reflect on Your Values and Goals: Consider what matters most to you in life and how you want to be treated in various medical scenarios. Think about what types of treatment align with your values and what you would want to avoid.
- Discuss with Loved Ones and Healthcare Providers: Have open and honest conversations with your family and healthcare providers about your wishes. This helps ensure that everyone understands your preferences and supports your decisions.
- Document Your Wishes: Write down your medical preferences in a clear and detailed manner. Use legal forms such as a living will or healthcare directive to formalize your plan.
- Choose a Healthcare Proxy: Select a trusted individual to act as your healthcare proxy or power of attorney for healthcare. This person should understand your values and be willing to advocate for your wishes.
- Review and Update Regularly: Revisit your advance care plan periodically and update it as needed, especially if your health status or personal preferences change.

Death literacy is about understanding and preparing for death in a way that respects the individual’s wishes and ensures a dignified passing. By fostering open discussions about death, educating healthcare providers, and supporting families, we can transform the end-of-life experience from one of fear and uncertainty to one of peace and dignity. Advance care planning is a proactive step toward ensuring that your end-of-life care reflects your values and desires. It provides peace of mind, reduces stress for your loved ones, and guides healthcare providers to deliver care that aligns with your wishes. By taking the time to create an advance care plan, you can ensure that you receive dignified and respectful care when it matters most. Death literacy is a critical step in ensuring that everyone has the right to a dignified and peaceful passing, honoring the beautiful journey of life to its end.