Only 4 percent of Indian Population has Access to Palliative Care
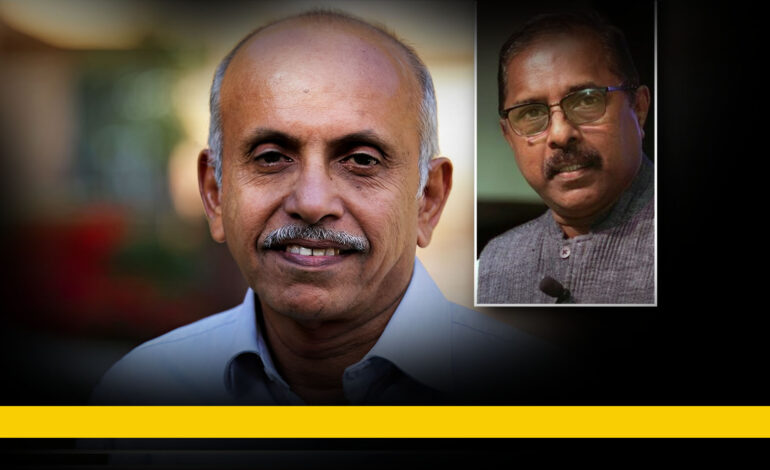
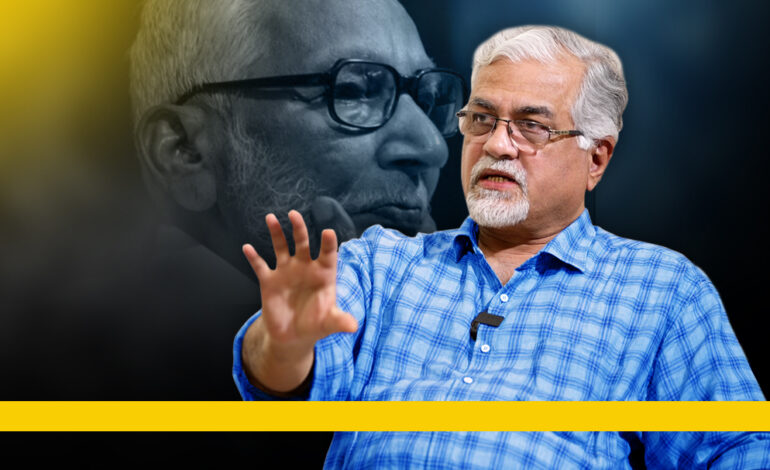
Along with the full text (in English) of the conversation between Dr. MR Rajagopal, the pioneering palliative care specialist in India and Dr. SS Lal, renowned public health care expert.
Dr Lal: Palliative care is a topic where a lot of discussions are happening in recent times. Today we are discussing this topic with a veteran in the field of palliative care, Dr MR Rajagopal, whom I personally view as one of my teachers. Dr Rajagopal has made very important interventions in the palliative care field in India.
Sir, Palliative care is often highly misunderstood as a care regime. I remember a doctor getting angry when his ailing wife was advised to be given palliative care. Even the medical community is not well-aware. So, my first question is very basic . What is Palliative Care?
Dr Rajagopal: We need a patient-centred approach in health care. As a medical student, I have seen many instances of patients suffering acute pain while others looked at it as a normal thing. Doctors and medical students who learn from them often prefer to turn their faces away from this pain. Now I understand that this reaction comes from a sort of helplessness. We did not know how to address this pain.
Dr Lal: As a child, I have also seen many patients suffer for days and months. Has the situation changed now? We all used to see pain just as an inevitable part of life. What do you think?
Dr Rajagopal: Only 4% of Indians have access to palliative care. 96% do not have access. Even the doctors who study MBBS and MD do not learn about pain relief. Palliative Care became part of our MBBS curriculum only in 2019.
Dr Lal: I also have felt that we are lacking something in our approach to pain. The common attitude is that we are destined to suffer pain.
Dr Rajagopal: Everybody compares other people’s pain to the pain that they have experienced sometime back in their lives. However, the other person’s pain could be more intense and we cannot know that. One might have experienced the pain of bone fracture or labour pain. Of the total palliative care needs of a society, only 30% is related to cancer. For example, Ischemic pain sometimes is far more unbearable than cancer pain. Sometimes the patient will suffer this pain for months or even years. Sometimes I feel there is this reluctance to address pain just because the solution is so simple. If expensive technology were involved, there would have been more interest for all. There is no glamour in this. This is not elite. Maybe that is the reason.
Dr Lal: Even now the public is not fully aware of the scope and importance of palliative care. Who can make them more aware? Do you think domain specialisation is a necessary prerequisite?
Medical Council of India has approved palliative medicine as a speciality even 7 years before it became part of MBBS curriculum. There are 10 centres in India and one in Kerala. Yet, there are only 30 palliative specialisation seats in these centres taken altogether. In a country of 1.3 billion population, we have only this many seats.
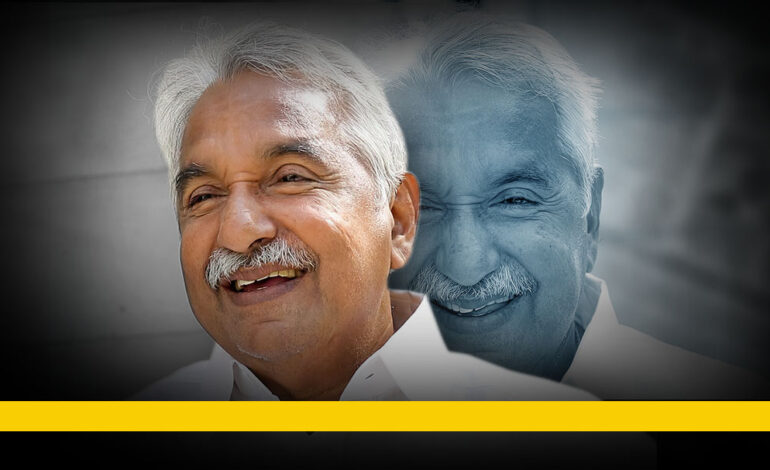
Dr Rajagopal: How effective has the government intervention been in educating the public about palliative care? No such intervention has been there from the government to educate the people. A National Programme for Palliative Care was instituted in 2012. Keshav Deshraj, the then Health Principal Secretary, had taken the initiative for that. That programme has a comprehensive approach in it. However, it was not implemented effectively. The National Health Policy of 2017 focused on instituting palliative care as part of primary health care. Under it, national level and state level trainers were trained during the Covid years. Now the policy has to be implemented by state governments.
Dr Lal: As you said, palliative medicine has become affordable for all. Yet, there are so many who do not have access to it. How can we fill in this gap in implementation?
Dr Rajagopal: There are huge gaps in implementation. For example, palliative care was included in the primary health sector. We all applaud that. But it is not there in tertiary care. Until someone’s disease is concluded as incurable, there is no provision for pain relief for the pain, for asthma, or depression that the patient suffers from. He or she has to reach the village in their last two weeks of life to get palliative care.
Isn’t that an irony? Doesn’t the care need to begin during the tertiary care days itself? Somehow, even the National Healthcare Policy is silent about tertiary sector palliative care. The World Health Organisation documents stress the need for palliative care in the primary sector. This is so because they already have palliative care in the tertiary sector. We mindlessly copied those guidelines.
In Kerala, the palliative policy was adopted in 2008. There was this problem in that too. The budget came from the National Rural Health Mission. So there was no specific budget allocated for the tertiary care sector. In 2019, when the policy was revised in Kerala, tertiary care was added. Due to Covid, its implementation is now delayed. Now the steps are being taken to implement in the tertiary sector.
The Kerala government has been very responsive to our demand to revamp the policy when we asked for it in 2019. Now budget allocation is required to implement the new policy. A few months before, some money was allocated to all Medical Colleges to start palliative units but the money has not reached the colleges yet as there were technical issues.
Dr Lal: In Kerala, the average longevity has increased. However, Kerala’s population has a high occurrence of lifestyle diseases and we do not have sufficient systems in place to support them when they need it. The kids who are abroad or working somewhere else come back for a few weeks for end of life care of their parents and the care is limited to it.
Dr Rajagopal: This is a very important issue. Ten percent of all of us including we two and the viewers of this interview will be dying from cancer. Seven percent of our population have dementia. According to India Population study 2015, 1.7 lakh aged persons were living alone. Of them, 1.43 lakh are women.
Dr Lal: Our culture is also contributing to that. In any marriage, men will be older than women on an average by 5 years. Added to that, men have less longevity than women here. So, they die at least 5 years younger and the age gap between a husband’s death and wife’s death thus is, on an average, 10 years. 10 years of widowhood thus becomes guaranteed.
Dr Rajagopal: As I said, out of the 1.7 lakh people who live alone, 1.43 lakh are women only. These are not the people who can afford a home nurse. In the villages, we, the palliative workers are familiar with the lives they live and the deaths they die. This is a big issue. We imported the idea of nuclear families from western countries. In the West, when they shifted to that family structure, they parallelly made systems to address the consequences; institutions such as nursing homes for the aged. We did not do that.
Dr Lal: Kerala has a huge geriatric population. The number of children per family is low and those kids would go to distant places to make a living. And we blame children for not looking after their parents in old age. However, the entire family sometimes would be living off his or her income only. Isn’t this a reality?
Dr Rajagopal: There is no meaning in blaming the children. Our generation created this kind of society where children are supposed to leave in search of better jobs. The average number of children per couple in Kerala is only 1.6. What happens is one couple shoulders the responsibility of looking after 4 aged persons. Don’t they have a life? Don’t they need to educate their own children? I will not blame the young generation. I have seen that most of them go that arduous extra mile to balance between their work and taking care of their parents.
Dr Lal: Another aspect is that in a family, it is the primary responsibility of women to care for the ailing and the aged. I know educated and employed women who take care of both their parents and in-laws. The burden is often entirely on women.
Dr Rajagopal: 90% of caregivers are women. The society here thinks that women are not supposed to live their own lives. Now the rich people have access to care homes but the poor cannot afford them. Care homes should be there and they have to be accessible to all.
Dr Lal: In Kerala, 60 to 70 percent of the population depend on the private sector for their health care needs. Care in the private sector incurs a heavy cost too. Do you think this has any impact on palliative care?
Dr Rajagopal: Among the audience of this interview, many would not like talking about death. Suppose somebody has the courage to talk about it and suppose we ask them, where they want to die; Is it among a number of machines, in an air conditioned ICU? Would you prefer it or would you want to die in your own bed? A large majority of those who go to private hospitals are now destined to die in intensive care units. Think what a cruel practice this is. When your life is ending, what would you want but a loving touch; I would want to say my last words to my wife, to hold the hands of my children, and to get a kiss on my cheek from my grandchildren. Instead you have tubes in all your orifices and you hear the bleeps of the machines when you die. There are many hurdles before us if we want to change this; there are legal ambiguities too. What is the responsibility of a doctor? There are many doctors who think that their responsibility is solely to prolong life in one way or the other. Medical science actually defines the role of a doctor as reducing suffering. The bio ethics unit of ICMR also says so. There is no understanding about the quality of life and death.
Dr Lal: Have you noticed this exploitative practice of falsely promising magical cures to people who have reached their end of life days and extracting their last savings? There are many such instances. I think that is an unavoidable tragedy. When you stand face to face with death, the first impulse is not to accept it.
Dr Rajagopal: Kubler-Ross who wrote the world famous book, ‘On Death and Dying’, has listed the different stages of grief. The first stage is denial. Then comes anger and the next is bargaining- you try to bargain with God praying that I will worship you if you let me live. The patient also bargains with his/her doctor- for example, if saved, they say they would never smoke again. Another kind of bargain is to blame it on the doctor treating that person and to approach another one- system hopping and doctor shopping. And there are many who try to exploit this situation.
Dr Lal: It has been an honour to do this interview because you are a person who has dedicated his life to palliative care and as a doctor myself, I respect you as a teacher too. Before we conclude, do you want to add anything as a message to our audience?
Dr Rajagopal: I would like to say this- palliative care is not just for cancer patients or for end-of-life care. It is the treatment regime to reduce suffering and pain in all kinds of ailments. As much as we understand that, the suffering of ourselves and the people who are around us gets reduced. We should also bring palliative care into the private sector.
Watch the full interview in Malayalam, here.
See more from MedTalk Series, Here.