Assisted Dying: The UK’s Misstep And Its Global Consequences

The British Parliament’s approval of the Assisted Dying Bill, allowing adults with a life expectancy of six months or less to seek medically assisted death, has sparked widespread debate. While this decision might seem like a step toward greater patient autonomy, its implications reach far beyond the UK. As a nation admired for its leadership in healthcare innovation and ethics, the UK’s actions influence developing countries like India and others in Africa and Asia, where healthcare challenges are even more profound.
This law risks sending the wrong message: that assisted dying is a viable “solution” to the suffering caused by systemic healthcare inadequacies. However, this approach is fraught with dangers, particularly for nations with limited resources and underdeveloped healthcare systems.
Lessons from Other Countries
The experiences of nations where assisted dying is legal reveal significant pitfalls that developing countries must heed:
- Expanding Criteria: In Belgium and the Netherlands, physician-assisted suicide has expanded to include non-terminal conditions like depression and dementia, and even socio-economic distress. This undermines the original intent of these laws. At many levels, this approach converts assisted dying into a sort of ill conceived solution for broader societal failures.
- Eroding Palliative Care: In Canada, where Medical Assistance in Dying (MAID) is legal, palliative care services and hospices are underfunded. For some, accessing death has become easier than accessing quality care—a troubling precedent.
- Pressure on the Vulnerable: In nations with legalized assisted dying, cases have emerged of individuals choosing death due to financial hardship or fear of being a burden. Such pressures could be even more pronounced in countries with high poverty and healthcare inequality.
These examples highlight the risks of normalizing assisted dying as an answer to suffering rather than addressing its root causes through better care and support.

Implications for Developing Countries
For nations like India, where millions lack access to even basic healthcare, let alone specialized palliative care, the legalization of assisted dying would exacerbate existing inequities:
- Disproportionate Impact on the Poor: In countries with fragile healthcare systems, the poor and marginalized are most likely to feel pressured to opt for assisted death, especially if palliative care options are unavailable.
- Stalled Progress in Palliative Care: Introducing assisted dying could divert resources and attention from developing essential palliative care services, leaving millions to suffer without adequate support.
- Erosion of Trust: When healthcare systems prioritize death over care, patients may lose trust in medical institutions, further complicating care delivery.
Legalizing assisted dying in these contexts risks normalizing death as a response to suffering rather than addressing the root causes of that suffering.
The UK’s Global Responsibility
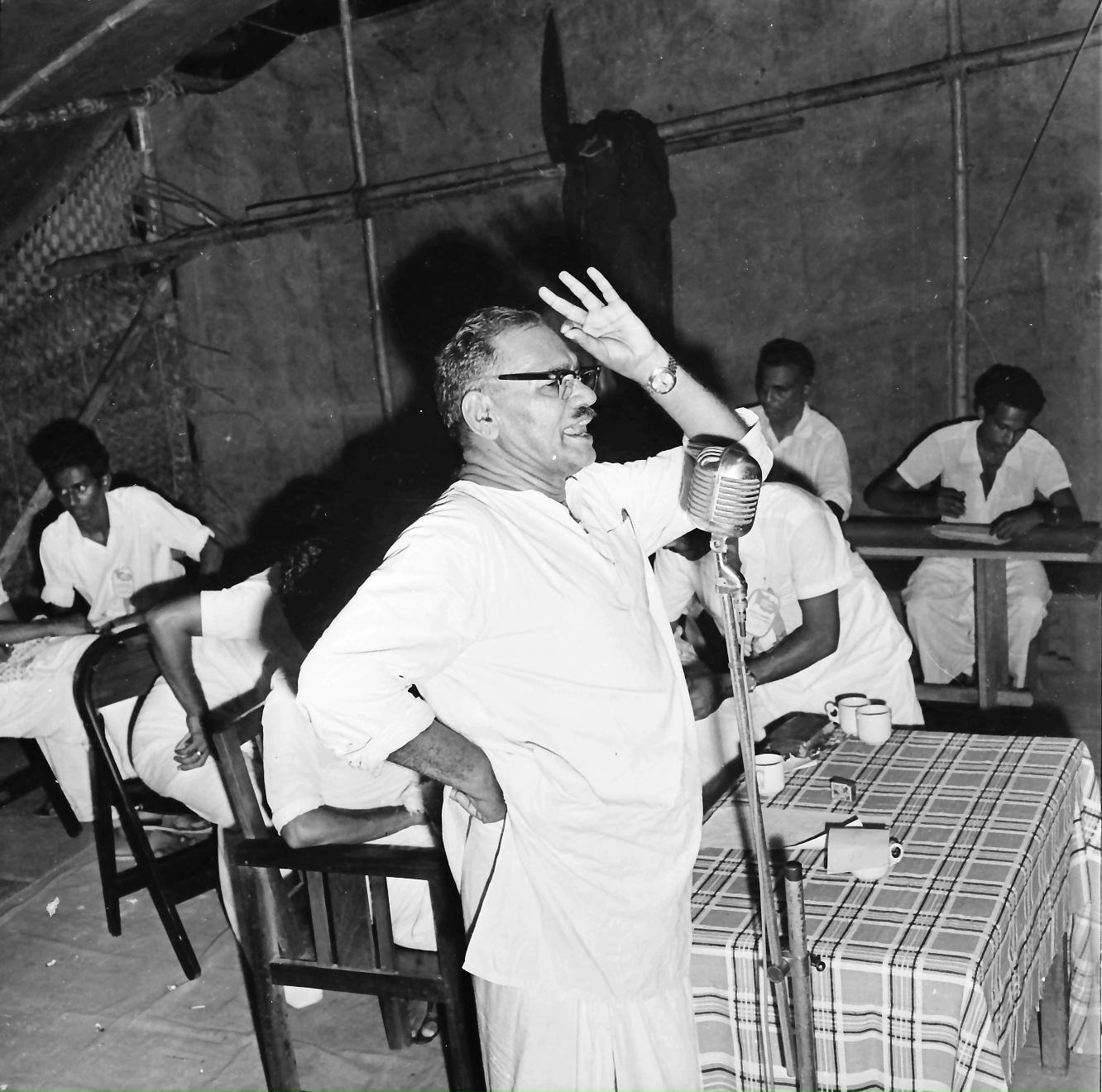
The UK has long been a leader in compassionate care, with institutions like St. Christopher’s Hospice pioneering modern palliative care. The passage of the Assisted Dying Bill has implications for this track record too. The minimum that the UK should do in this context is that it must ensure that this does not overshadow its legacy of prioritizing life-affirming care. The UK has a moral responsibility to champion palliative care globally and prevent the misuse of assisted dying as a substitute for genuine support.

A Call to Action
Rather than advocating for physician-assisted suicide, developing nations need a global commitment to strengthening palliative care systems. Organizations like the World Health Organization (WHO) have emphasized that palliative care is a critical component of universal health coverage. To that end, countries like the UK can:
1.Support Palliative Care Research and Training: Provide expertise and resources to help developing nations build robust palliative care frameworks.
2.Promote Ethical Healthcare Policies: Ensure that debates on assisted dying also focus on addressing inequalities in healthcare access.
3.Lead by Example: Emphasize compassionate care and holistic support, demonstrating that autonomy and care can coexist without resorting to assisted dying as a default option.
The True Measure of Progress
Legalizing assisted dying may appear progressive, but real progress lies in ensuring that no one is forced to choose death due to inadequate care or poverty. The UK must balance its decision with a renewed commitment to compassionate, patient-centered care—setting an example that the world, particularly developing nations, can follow.